HEALTH 3.0 VISION
― Winston S. Churchill
Health 3.0 Vision
Taking the best aspects of 1.0 (deep sacred relationships, physician autonomy) and the key pieces of 2.0 (technology, evidence, teams, systems thinking), Health 3.0 restores the human relationship at the heart of healing while bolstering it with a team that revolves around the patient while supporting each other as fellow caregivers. What emerges is vastly greater than the sum of the parts.
Caregivers and patients have the time and space and support to develop deep relationships. Providers hold patients accountable for their health, while empowered patients hold us accountable to be their guides and to know them—and treat them—as unique human beings. Our EHRs bind us and support us, rather than obstruct us. The promise of Big Data is translated to the unique patient in front of us. Our team provides the lift so everything doesn’t fall on one set of shoulders anymore (health coaches, nurses, social workers, lab techs, EVERYONE together). We are evidence-empowered but not evidence-enslaved. We are paid to keep people healthy, not to click boxes while trying to chase an ever-shrinking piece of the health care pie. Our administrators seek to grow the entire pie instead, for the benefit of ALL stakeholders.
As I’ve shared this framework, I’ve received a couple of questions/comments to the effect of “where’s insurance?” It’s not here as it’s not about who is assuming the financial risk. That varies by country and, even in the U.S., most risk is assumed by employers or various government entities at the state and federal level. The “insurance” companies are largely claims processors (typically only about one-third of the claims insurance companies process are their funds at risk). No matter who carries the risk, we’re bad at purchasing health care and health & wellness services in the U.S. This framework suggests we need to take a fresh look, rather than buying what has been radically underperforming.
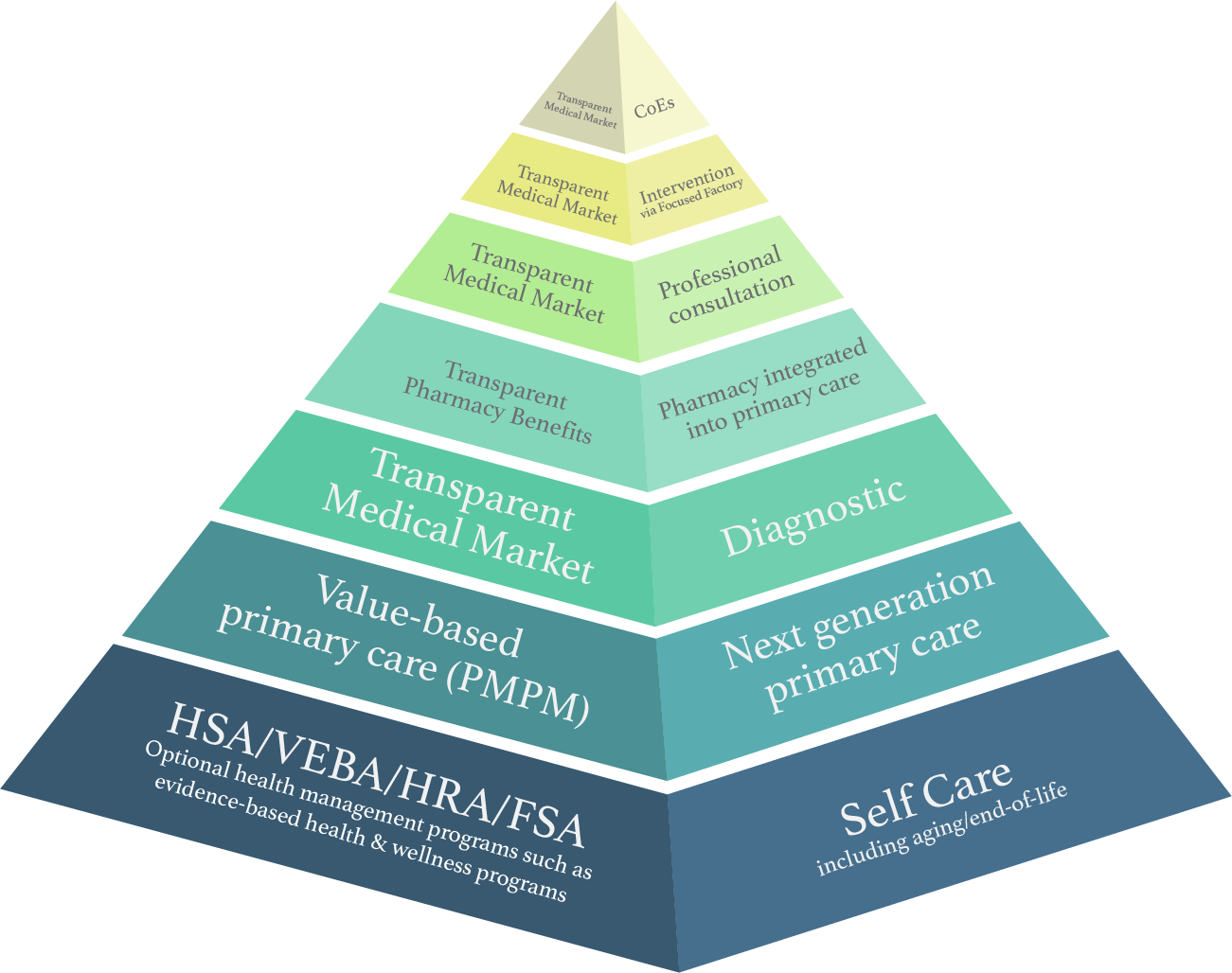
The pyramid graphic below is the start of developing a North Star for how various elements of health and health care interrelate with each other. It’s going to require some verbal explanation of where we’re going with this. The “we” is Dr. Venu Julapalli, Dr. Zubin Damania (aka ZDoggMD), Jonathan Bush, and Dr. Vinay Julapalli. The problem we’re trying to address is how health care is “organized” in a tangled jumble of silos largely organized around medical technologies, not individuals (patients). It’s exacerbated by economic models and information technology that further impair healing. We believe that fostering an ecosystem that is antifragile should be one of the key design points.154 Flawed thinking looks at health care simply as an expense (or, from the perspective of the health care industry, revenue to be maximized). As Churchill states, when health is looked at as an asset, it causes one to optimize for something completely different.
For those unfamiliar with Nassim Taleb’s book, Antifragile, he introduces the book as follows:
Some things benefit from shocks; they thrive and grow when exposed to volatility, randomness, disorder, and stressors and love adventure, risk, and uncertainty. Yet, in spite of the ubiquity of the phenomenon, there is no word for the exact opposite of fragile. Let us call it antifragile. Antifragility is beyond resilience or robustness. The resilient resists shocks and stays the same; the antifragile gets better.
Health care has been unique in that it uses technology as an excuse for costs to go up and productivity to go down. In Health 3.0, a properly organized health ecosystem can benefit from technology rather than helping fuel hyperinflation for all of us, while decreasing productivity and job satisfaction for clinicians.
Figure 14 is a thumbnail sketch for how the pyramid works. You can also explore an interactive graphic at healthrosetta.org/ health30. Each layer represents a level of care or self-care. You want to spend as much of your life as possible in self-care at the bottom of the pyramid.* When you have to move to higher layers, you want to move back down asap.
Each pyramid layer has four facets, one for each side of the pyramid.
- Optimal way to deliver health services
- Optimal way to pay for care
- Enabling technology for #1 & #2
- Enabling government role for #1 & #2
Following a given layer (e.g., value-based primary care 3.0) shows how the four facets apply to that layer.
You read the pyramid from the bottom and at each layer look at the four facets to ensure they are meeting your goals. Thus, you would see that the self-care layer is at the bottom. When you access the health care system next generation primary care is where you should start. In places like Denmark and the best value-based primary care organizations in the U.S., over 90 percent of care can be addressed in a proper primary care setting. Full valued-based primary care includes things like behavioral health, interior work, health coaches, and physical therapy, all enabled by technology like secure messaging, remote monitoring, and other future advances.
Chapter 14 covers value-based primary care and focuses on high-cost individuals who consume the vast majority of health care spending. For the majority of people who have simpler primary care needs, there are more streamlined, technology-enabled, and cost-effective methods of delivery. For example, Dr. Jay Parkinson has proposed what he calls “Primary Care 3.0” which is optimized for the majority of people with simple medical needs.
If an issue can’t be addressed in primary care, you move up to the diagnostic layer (e.g., lab tests) for deeper insight to rule in/out various issues. Then, if you need a prescription, you’d go to the next layer―pharmacy woven into primary care. Organizations such as ChenMed do this well. If a prescription isn’t the answer, you proceed to the next layer for a “professional consultation”. This is a consult between the PCP and an unconflicted specialist. In this context, unconflicted means that the specialist wouldn’t be performing an intervention or procedure, thus removing the profit incentive to overtreat. If an intervention is needed, you proceed to the next layer―intervention via focused care setting with deep experience in the intervention.
Jonathan Bush, CEO of athenahealth, told me about his own knee surgery and finding that even the highest-volume knee surgeons in Boston only do less than one-third of what they could. They spend the rest of their time doing a bunch marketing they’d rather not do (e.g., be a “team doctor” for a sports team to market themselves). Most would rather spend the majority of their time doing what they do best. If they did, they could drop their unit price.
Finally, for the unfortunate few who have rare and highly complex conditions, they’d go to a Center of Excellence (CoE) in their condition like the NIH, Mayo, etc. at the top of the pyramid.
To reiterate, even when at higher levels of the pyramid, the goal is to move back down the pyramid as soon as possible.
As I developed this framework further, I was interested in getting specialists’ feedback. Relatively speaking, I’ve spent more time with primary care physicians at the base of the pyramid. The most advanced and successful value-based primary care organizations intuitively understand two key issues that drive costs and quality.
- Fostering self-care and caregiving by nonprofessional loved ones is essential to optimizing healing and health.
- Without a seasoned “ship captain” (the primary care physician), rough medical seas cause patients to needlessly suffer from an uncoordinated health care system.
Specialists, like any group of humans, have many opinions, but I will share the feedback from Dr. Venu Julapalli on the framework (he has also been writing about the tenets of Health 3.0).156 The following are Dr. Julapalli’s comments, edited for length and clarity.
I am loving what you guys have come up with.
- It starts with self-care at the base. That’s key. It underscores personal responsibility in health, which has been woefully neglected. At the same time, social determinants of health (SDoH) are right at the base, where they belong. I love the pyramid’s government facet, letting it act as the market accelerator, not an overly active market participant without the ability to enable the most effective and efficient system.
- It properly puts value-based primary care right near the base. As a specialist, I don’t need to be near the base. I also need to have as few conflicts of interest as possible in my interactions with primary care.
- It properly puts the specialist care in focused settings near the top (this position doesn’t make them the most important, just the most focused). This is what Devi Shetty is executing in India and Cayman Islands―high-volume cardiovascular surgery by experts who love what they do, while dropping unit price ridiculously through streamlined operations and economies of scale.
- It appropriately puts Centers of Excellence at the very top―go there for help with rare diagnoses, but keep it limited. We should also never forget the power of the engaged patient, who destroys the most expert doctors when love for life takes over. See this article as an example, “His Doctors Were Stumped. Then He Took Over.”
Overall, I love this pyramid framework. Conceptually, it’s honoring much of what I’ve come to believe on health care, health, and healing. You’re distilling what real-life experiences and data have shown works in health care.
I will conclude with a quote highlighting how we need a major overhaul. Simply shifting who pays is just moving deck chairs on the Titanic. Metaphorically, we’re all on the same ship. Dr. Otis Brawley, chief medical officer for the American Cancer Society said, “I have seen enough to conclude that no incident of failure in American medicine should be dismissed as an aberration. Failure is the system.”